
Menopause
What is the menopause?
Menopause or cessation of menstrual cycles is a normal part of a woman’s life. The diagnosis of menopause is made after 12 months of amenorrhoea.3
Menopause is a natural phenomenon after which periods stop permanently. It is a retrospective diagnosis detemined after 12 consecutive months without menses and when no other biological or physiological cause can be identified.3 Menopause may affect the woman’s quality of life and has both physiological and psychological effects.7
What do we have in common?
We all go our own way.
When does menopause start?
The menopause is a natural part of ageing that usually occurs between 45 and 55 years of age, as a woman's estrogen levels decline. In the UK, the average age for a woman to reach the menopause is 51.7
Some women may experience premature ovarian insufficiency (POI), which is when the menopause occurs at the age of 40 or earlier and may be associated with other underlying medical conditions (e.g. surgical menopause). Menopause occurring earlier in life, can also be linked to underlying pathological conditions such as ovarian cancer, breast cancer and adverse effects of cancer treatment modalities such as chemotherapy and radiotherapy and hormonal imbalances in the body.8
What is the physiology of menopause?
During the female reproductive life cycle, oocytes in the ovaries undergo atresia, which in turn results in an overall depletion of the follicles. Hormonal fluctuation is also evident during the menopausal transition period. As the age advances, fertility of women starts to decline and chances of becoming pregnant are reduced to a greater extent.1,2
The stages of the menopause
Perimenopause: The time in which a woman has irregular cycles leading up to menopause and continuing until 12 months after her final period.3
Menopause: A biological stage in a woman’s life that occurs when she stops menstruating and reaches the end of her natural productive life.3
Postmenopause: The time after menopause has occurred, starting when a woman has not had a period for 12 consecutive months.3
Physiological changes during menopause
The first evident hormonal change during perimenopause is an increase in the pituitary gonadotropin follicle stimulating hormone (FSH) levels, which is associated with a decrease in the gonadotropin-sensitive ovarian follicles.2 The development of follicles during perimenopause is erratic, which leads to excessive production of FSH by the pituitary gland, thereby stimulating the resistant follicles.1 A fluctuation in the levels of estrogen, progesterone and inhibin are also observed during this transition period. The levels of FSH and estrogen during perimenopause can differ from one woman to another.6
What are the symptoms of menopause?
During menopausal transition, women often experience a wide range of symptoms – the common symptoms being hot flushes, night sweats, insomnia, mood changes, body fat changes and vaginal bleeding disorders due to change in the levels of estrogen and FSH.
Other symptoms that may be observed include urogenital atrophy, vaginal dryness, feeling of bloating and headaches.1,2,4,9
However, menopausal symptoms may vary from one individual to another. The symptoms may begin years before and continue for a variable duration after the final period.6
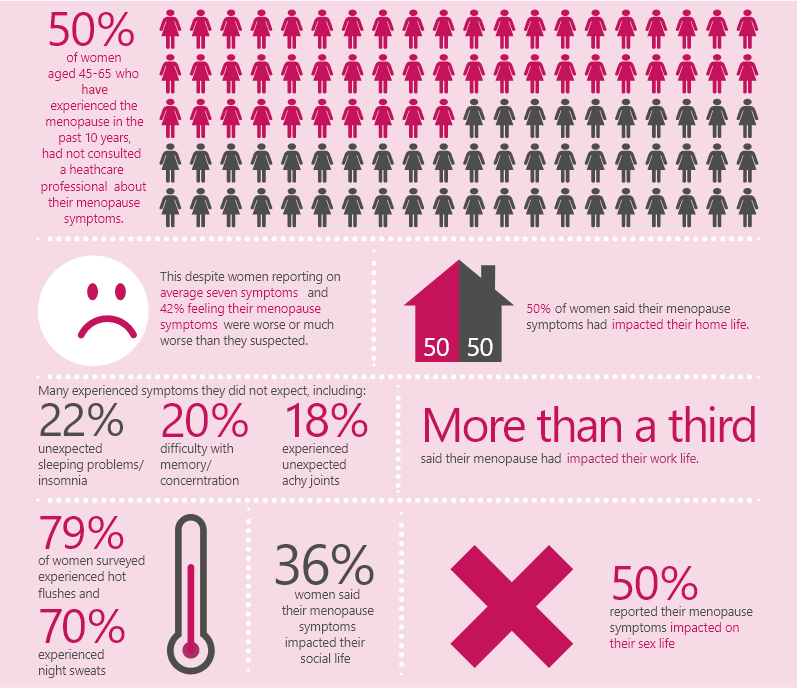
Adapted from: The British Menopause Society, National Survey 2016. Accessed from: https://thebms.org.uk/publications/tools-for-clinicians/. Last accessed September 2021.
How is menopause diagnosed?
Diagnose the following without laboratory tests in otherwise healthy women aged over 45 years with menopausal symptoms: perimenopause based on vasomotor symptoms and irregular periods, menopause in women who have not had a period for at least 12 months and are not using hormonal contraception, menopause based on symptoms in women without a uterus.3
Take into account that it can be difficult to diagnose menopause in women who are taking hormonal treatments, for example for the treatment of heavy periods.3
Do not use the following laboratory and imaging tests to diagnose perimenopause or menopause in women aged over 45 years: anti-Müllerian hormone, inhibin A, inhibin B, estradiol, antral follicle count or ovarian volume.3
Do not use a serum follicle stimulating hormone (FSH) test to diagnose menopause in women using combined estrogen and progestogen contraception or high-dose progestogen.3
Consider FSH test to diagnose menopause only: in women aged 40 to 45 years with menopausal symptoms, including a change in their menstrual cycle or in women aged under 40 years in whom menopause is suspected.3
What are the risks and complications associated with menopause?
Menopausal transition is associated with hormonal fluctuations, thereby predisposing menopausal women to symptoms such as urinary incontinence, polyuria, vaginal dryness leading to discomfort during sexual intercourse, and an increased risk of osteoporosis and cardiovascular disease.1,2,5
What are the treatment options for menopause?
Offer women HRT for vasomotor symptoms after discussing with them the short-term (up to 5 years) and longer-term benefits and risks. Offer a choice of preparations as follows:3
- Estrogen and progestogen to women with a uterus
- Estrogen alone to women without a uterus
Do not routinely offer selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs) or clonidine as first-line treatment for vasomotor symptoms alone.3
Explain to women that there is some evidence that isoflavones or black cohosh may relieve vasomotor symptoms. However, explain that:3
- Multiple preparations are available and their safety is uncertain
- Different preparations may vary
- Interactions with other medicines have been reported
-
References
- 1) Butler L, Santoro N. The reproductive endocrinology of the menopausal transition. Steroids. 2011 Jun;76(7):627-35.
- 2) Santoro N, Randolph JF. Reproductive hormones and the menopause transition. Obstet Gynecol Clin North Am. 2011 Sep;38(3):455-66.
- 3) NICE. Menopause: diagnosis and management. NG23. Available at: www.nice.org.uk/guidance/ng23 (accessed September 2021).
- 4) Cohen LS, Soares CN, Joffe H. Diagnosis and management of mood disorders during the menopausal transition. Am J Med. 2005 Dec;118(12):93-7.
- 5) Finkelstein JS, Brockwell SE, Mehta V, et al. Bone mineral density changes during the menopause transition in a multiethnic cohort of women. J Clin Endocrinol Metab. 2008 Mar;93(3):861-8.
- 6) Harlow SD, Gass M, Hall JE etal; STRAW+ 10 Collaborative Group. Executive summary of the Stages of Reproductive Aging Workshop+ 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012 Apr;97(4):1159-68.
- 7) NHS. Menopause overview. Available at https://www.nhs.uk/conditions/menopause/#:~:text=The%20menopause%20is%20a%20natural,before%2040% 20years%20of%20age. Last accessed: September 2021.
- 8) NHS. Early menopause. Available at https://www.nhs.uk/conditions/early-menopause/. Last accessed: September 2021.
- 9) Davis SR, Castelo-Branco C, Chedraui P et al. Understanding weight gain at menopause. Climacteric. 2012 Oct;15(5):419-29.
Femoston®
Femoston is a combination of 17β estradiol and dydrogesterone, which is indicated for postmenopausal women at least 6 months since last menses to provide relief from vasomotor symptoms.

WHAT ARE THE EXPERTS SAYING?
Watch our menopause experts discuss the benefits of an individualised approach when it comes to HRT treatment.
HCP Disclaimer
This website is intended for UK healthcare professionals only.
Viatris Connect is an online platform for UK healthcare professionals.
Across the website you will find news, blogs and product information.
FREE Menopause and HRT webinars available to watch by registering to Viatris Connect today
Please note that the website contains promotional and non-promotional material including educational content and resources to help you and your patients.
REGISTER NOW








